Digestive System, Bowel Control, Constipation, and Fecal Incontinence
How we get nutrition and how we eliminate waste is usually taken for granted until there is a problem with the system. The digestive system begins at the mouth and ends at the anus. Here is an overview of the parts that make up the digestive system and how each works within this complex system.
Mouth
- Ingests food/fluid
- Breaks food down by chewing
- Begins digestion by adding saliva
Esophagus
- This tube carries food/fluid to the stomach
Stomach
- Breaks down and mixes up food
- Holds food until the bowel is ready for it (up to two hours)
- Can hold one liter of food and fluid (we feel full with 1/2 liter)
Gastrocolic Reflex
- Initiates peristaltic waves (muscle contractions) of digested food onward to rectum 3-6 times a day via the pyloric sphincter
Small Intestines (Bowel)
- Has the duodenum, where most digestion takes place because of added secretions from the pancreas, gallbladder, liver, jejunum, then ilium
- Takes 4-6 hours for food to go through this section
Colon (Large Intestine)
- Receives 1000-1500 ml of digested food, which is now a thick liquid, per day
- Has three parts: ascending colon, transverse colon and the descending colon
- Transit time through the colon from the ascending colon, transverse colon, and descending colon to the sigmoid (storage) is 24-72 hours depending on what has been eaten; fatty meals take longer
- Passes along hardened feces to the rectum
Rectum
- Once stool enters into the rectum we become aware that we need to have a bowel movement.
How Food Passes Through the Digestive System
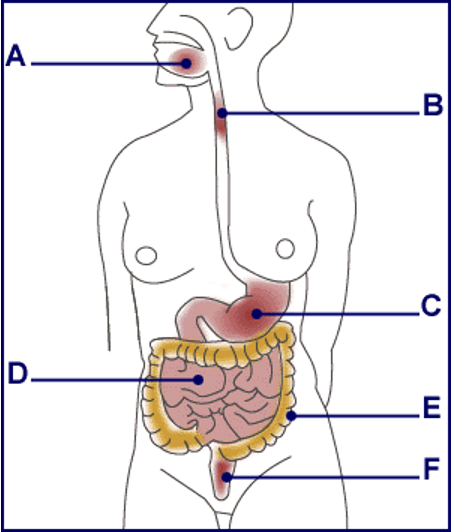
A. Mouth: Food is chewed in the mouth. This takes up to one minute.
B. Esophagus: Food is swallowed, taking three seconds to pass through the esophagus.
C. Stomach: Digestion starts in the stomach, where food stays for 1-3 hours.
D. Small Intestine: Liquidized food takes about 2-6 hours to travel through the small intestine. By now it is fully digested.
E. Large Intestine: By the end of its stay in the large intestine (12-48 hours), most of the water content has been absorbed (about 1 qt).
F. Rectum: Stools and gas are stored in the rectum until they are expelled through the anus.
Image from http://www.continence-foundation.org.uk
Introduction to Bowel Health
Diet and daily habits can help you predict when your bowels will move on a regular basis. The consistency and quantity of the stool is usually more important than the frequency. The goal is to have a regular bowel movement that is soft but formed. “Normal” frequency is 3/day-3/wk.
Tips on Emptying Regularly
- Eat breakfast. Usually the best time of day for a bowel movement will be a half hour to an hour after eating. These times are best because the body uses the gastrocolic reflex, a stimulation of bowel motion that occurs with eating, to help produce a bowel movement. For some people even a simple hot drink in the morning can help the reflex action begin.
- Eat all your meals at a predictable time each day. The bowel functions best when food is introduced at the same regular intervals.
- The amount of food eaten at a given time of day should be about the same size from day to day. The bowel functions best when food is introduced in similar quantities from day to day. It is fine to have a small breakfast and a large lunch, or vice versa, just be consistent.
- Eat two servings of fruit or vegetables and at least one serving of a complex carbohydrates (whole grains such as brown rice, bran, whole wheat bread, or oatmeal) at each meal.
- Drink plenty of water—ideally 4+ glasses a day. Be sure to increase your water intake if you are increasing fiber into your diet.
Maintain Healthy Habits
- Exercise daily. You may exercise at any time of day, but you may find that bowel function is helped most if the exercise is at a consistent time each day.
- Make sure that you are not rushed and have convenient access to a bathroom at your selected time to empty your bowels.

Introduction to Fiber
Fiber Overview
Dietary fiber is the part of plants that can’t be digested. There are 2 kinds of dietary fiber: insoluble and soluble. Insoluble fiber adds bulk to keep foods moving through the digestive system. Soluble fiber holds water, which softens the stool for easy bowel movements. Fiber is an important part of your diet, even though it passes through your body undigested and has no nutritional value. A high fiber diet can:
- promote regular bowel movements
- treat diverticular disease (inflammation of part of the intestine) and irritable bowel syndrome (abdominal pain, diarrhea, and constipation that come and go)
- promote improvement in hemorrhoids, constipation and fecal incontinence
You should have at least 14 grams of fiber for every 1000 calories you eat every day. Read the label on every food package to find out how much fiber a serving of the food will provide. Foods containing more than 20% of the daily value of fiber per serving are considered high in fiber.
Without enough fiber in your diet, you may suffer from:
- constipation
- small, hard, dry bowel movements.
Sources of Fiber
Breads, cereals, and pasta made with whole grain flour, and brown rice are high fiber foods. Many breakfast cereals list the bran or fiber content, so it’s easy to know which products are high in fiber.
All fruits and vegetables also contain fiber. Dried beans, leafy vegetables, peas, raisins, prunes, apples, and citrus fruits are all especially good sources of fiber. Additional information on fiber content in foods is available at www.caloriecounts.com
Types of Fiber
There are two main types of fiber: insoluble and soluble. Both of these types can prevent and relieve constipation and diarrhea, although some people find one or the other to be more easily digested.
Insoluble Fiber
Functions of Insoluble Fiber
- moves bulk through the intestines
- controls and balances the pH (acidity) in the intestines
Benefits of Insoluble Fiber
- promotes regular bowel movement and prevents constipation
- removes fecal waste through colon in less time
- keeps an optimal pH in intestines to prevent microbes from producing cancer substances, therefore preventing colon cancer
Food Sources of Insoluble Fiber
- whole-wheat products
- wheat bran “miller’s bran”
- corn bran
- flax seed or other seeds
- vegetables such as green beans, broccoli, cauliflower and potato skins
- fruit skins and root vegetable skins
- popcorn
- brown rice
Soluble Fiber
Functions of Soluble Fiber
- holds water in the colon to bulk and soften the stool
- prolongs stomach emptying time so that sugar is released and absorbed more slowly
Benefits of Soluble Fiber
- lowers total cholesterol and LDL cholesterol (the bad cholesterol) therefore reducing the risk of heart disease
- regulates blood sugar for people with diabetes
Food Sources of Soluble Fiber
- oat/oat bran
- dried beans and peas
- nuts
- barley
- flax seed or other seeds
- fruits such as oranges, pears, peaches, and apples
- vegetables such as carrots
- psyllium husk
- prunes
Adding Fiber to Your Diet
Eating foods that are high in fiber can help relieve some problems with constipation, hemorrhoids, diverticulitis and irritable bowel syndrome. A high-fiber diet can provide long-term health benefits. Here are some tips to help you easily add fibers to your diet.
Start Slowly!!
Many people notice bloating, cramping or gas when they add fiber to their diet. Making small changes in your diet over a period of time can help prevent this. Start with one of the changes listed below, then wait several days to a week before making another. If one change doesn’t seem to work for you, try a different one. You may have some gas or bloating at first, but your body will adjust in time.
It’s important to drink more fluids when you increase the amount of fiber you eat. Try for at least 1-2 more glasses of water a day when you increase your fiber intake.
Tips for Increasing Fiber
- Start your day with a high-fiber breakfast cereal. Check labels on the packages for the amounts of dietary fiber in each brand.
- Eat at least 5 servings of fruits and vegetables each day. Fruits and vegetables that are high in fiber include:
- Apples, Berries, Oranges
- Broccoli, Cauliflower, Green Peas
- Pears, Prunes, Figs
- Brussel Sprouts, Carrots, Beans
- Include fruits or vegetables with every meal. Use carrot sticks or apple slices for snacks.
- Cooked fiber is just as effective as raw fiber, so incorporate high-fiber foods in your cooking.
- When preparing food leave edible skins and seeds, and use whole-grain flours.
- Serve fruit-based desserts.
- Replace white bread with whole-grain breads and cereals. Eat brown rice instead of white rice.
- Eat more of the following foods:
| Bran muffins Brown rice | Oatmeal Popcorn | Multiple-grain cereals, cooked or dry 100% whole-wheat bread |
- Add whole grains and dried beans to casseroles.
- Add a couple TBSP wheat bran, flaxseed meal, or chia seeds to cereals or baking; ¼ c bulgur wheat to meat loaf or to extend 1 lb ground beef.
If you still suffer from constipation, talk to your health care provider about fiber laxatives. Psyllium (Metamucil, Kosyl), Benefiber, or Citrucel are soluble fibers that are often used for this purpose. However, when you tend towards constipation, too much of these can stop you up more. They can be taken in tablet form or as a powder that is mixed in a glass of water. Always read and follow the directions on the label carefully. Talk to your doctor or pharmacist if you have any concerns about fiber.
Fiber Table — Grams of Fiber in Food
For additional information on fiber content in foods, go to www.caloriecounts.com
| Food Products | Serving Size | Grams of Fiber/serving |
| Breads | ||
| Whole Wheat | 1 slice | 2.11 |
| White | 1 slice | 0.5 |
| Rye | 1 slice | 1.72 |
| Cereals | ||
| Oat Bran | 1 oz. | 4.06 |
| Wheat Bran | 1 oz. | 10.0 |
| All Bran | ½ cup | 6.0 |
| Optimum | 1 cup | 10.0 |
| Whole Wheat Total | 1 cup | 3.0 |
| Fiber One | ½ cup | 13.0 |
| Shredded Wheat | 1oz. | 2.64 |
| Corn Flakes | 1 oz. | 0.45 |
| Cheerio’s | 1 1/3 cup | 2.0 |
| Oatmeal | 1 oz. | 2.5 |
| Rice | ||
| Brown | ½ cup | 5.27 |
| White | ½ cup | 1.42 |
| Spaghetti | 2 oz. | 2.56 |
| Vegetables (cooked) | ||
| Broccoli | ½ cup | 2.58 |
| Brussels sprouts | ½ cup | 2.0 |
| Cauliflower | ½ cup | 2.6 |
| Carrots | ½ cup | 3.2 |
| Corn | ½ cup | 3.03 |
| Eggplant | ½ cup | 0.96 |
| Green peas | ½ cup | 3.36 |
| Lettuce (raw) | ½ cup | 0.24 |
| Baked potato w/skin | ½ cup | 2.97 |
| Spinach | ½ cup | 2.07 |
| Squash | ½ cup | 2.87 |
| Tomato (raw) | ½ cup | 1.17 |
| Zucchini | ½ cup | 1.26 |
| Beans | ||
| Green (canned) | ½ cup | 1.89 |
| Kidney | ½ cup | 5.48 |
| Lima | ½ cup | 4.25 |
| Pinto | ½ cup | 5.93 |
| Fresh fruits | ||
| Apple (with peel) | 1 medium | 2.76 |
| Apricots | 1 cup | 3.13 |
| Banana | 1 medium | 2.19 |
| Black/Boysenberries | 1 cup | 7.2 |
| Grapefruit | 1 medium | 3.61 |
| Grapes | 1 cup | 1.12 |
| Nectarine | 1 medium | 2.2 |
| Orange | 1 medium | 3.14 |
| Pear (with peel) | 1 medium | 4.32 |
| Prunes | 3 | 3.5 |
| Raspberries | 1 cup | 7.5 |
| Strawberries | 1 cup | 3.87 |
| Watermelon | 1 slice | 1.93 |
About Constipation
Constipation Overview
- Constipation is the most common gastrointestinal complaint — about 4 million Americans experience constipation and make 2.5 million physician visits a year to get help for the problem. Constipation can occur when the colon absorbs too much water, the colon’s muscle contraction is slow or sluggish, and/or there is delayed transit time through the colon. The result is stool that is hard and dry. Indicators of constipation include straining during bowel movements greater than 25% of the time, having fewer than three bowel movements per week, and/or the feeling of incomplete evacuation.
- There are established guidelines (Rome II ) for defining constipation. A person needs to have two or more of the following symptoms for at least 12 weeks (not necessarily consecutive) in the preceding 12 months:
- Straining in greater than 25% of bowel movements
- Lumpy or hard stools in greater than 25% of bowel movements
- Sensation of incomplete emptying in greater than 25% of bowel movements
- Sensation of anorectal obstruction/blockade in greater than 25% of bowel movements
- Manual maneuvers to help empty greater than 25% of bowel movements (e.g., digital evacuation, support of the pelvic floor)
- Less than 3 bowel movements/week
- Loose stools are not present, and criteria for irritable bowel syndrome are insufficient
Common Causes of Constipation
- Lack of fiber in your diet
- Lack of physical activity
- Medications, including iron and calcium supplements
- Dairy intake
- Dehydration
- Abuse of laxatives
- Travel
- Irritable Bowel Syndrome
- Pregnancy
- Luteal phase of menstruation (after ovulation and before menses)
- Colorectal problems
- Intestinal dysfunction
Treating Constipation
There are several ways of treating constipation, including changes to diet and exercise, use of laxatives, adjustments to the pelvic floor, and scheduled toileting. These treatments include:
- Increasing fiber and fluids
- Increasing physical activity
- Learning muscle coordination
- Learning proper toileting techniques and toileting modifications
- Designing and sticking to a toileting schedule
- Use miralax as needed to soften stoo
Laxatives
Natural:
- Prunes (4-5 once or twice a day), Pears, apples, kiwi
- Prune or pear juice, apple cider (unfiltered if possible) with pulp
- 1c oat bran, 1 c unsweetened applesauce, ½ c prune juice- mix together and have 2 tsp-6 TBSP daily with AT LEAST 8 oz water
- Oatmeal, granola, Bran buds
- Coffee- can help stimulate bowel function (hot water can work, too)
- Water- need at least 1 qt a day to keep enough water in the stool. If you don’t drink enough water with additional fiber, it can turn to concrete in your colon!
- Activity- walking and moving around helps to stimulate normal muscle contractions through the intestines
Supplements: (table adapted from mayoclinic.org)
| Type of laxative | How it works | Side affects |
| Osmotic (Miralax, milk of magnesium) | Draws water into colon to soften stools | Bloating, cramping, diarrhea Miralax may take 3-5 days to act |
| Bulking agents (Benefiber, Metamucil, Citrucel, Fibercon) | Absorb water to form soft, bulky stools. Promotes normal muscle contractions. | Bloating, gas, can be constipating if not balanced with enough water. |
| Stool softeners (Colace) | Adds water to stool to soften. | Electrolyte imbalance if prolonged use |
| Stimulants (Senokot, Dulcolax, ExLax) | Stimulates contractions of intestinal muscles. Can also soften stools. | Can be habit forming over time. Cramping, diarrhea. |
Toileting Techniques for Bowel Movements (Defecation)
Using your belly (abdomen) and pelvic floor muscles to have a bowel movement is usually instinctive. Sometimes people can have problems with these muscles and have to relearn proper defecation (emptying) techniques. If you have weakness in your muscles, organs that are falling out, decreased sensation in your pelvis, or ignore your urge to go, you may find yourself straining to have a bowel movement. You are straining if you are:
- holding your breath or taking in a huge gulp of air and holding it
- keeping your lips and jaw tensed and closed tightly
- turning red in the face because of excessive pushing or forcing
- developing or worsening your hemorrhoids
- getting faint while pushing
- not emptying completely and have to defecate many times a day
If you are straining, you are actually making it harder for yourself to have a bowel movement. Many people find they are pulling up with the pelvic floor muscles and closing off instead of opening the anus. Due to lack of pelvic floor relaxation and coordination the abdominal muscles, one has to work harder to push the feces out.
Many people have never been taught how to defecate efficiently and effectively. Notice what happens to your body when you are having a bowel movement. While you are sitting on the toilet pay attention to the following areas:
- Jaw and mouth position
- Angle of your hips
- Whether your feet touch the ground or not
- Arm placement
- Spine position
- Waist
- Belly tension
- Anus (opening of the anal canal)
There is a good YouTube video on “How to Empty your Bowels without Straining” by Michele Kenway
How to poop! Here are the 4 basic points:
- Lean forward enough for your elbows to rest on your knees
- Support your feet on the floor or use a low stool if your feet don’t touch the floor
- Push out your belly as if you have swallowed a beach ball—you should feel a widening of your waist, and then tighten the belly and push (“belly big, belly hard”)
- Open and relax your pelvic floor muscles, rather than tightening around the anus
- Sit on the toilet
- Make sure your feet are supported.
- Notice your hip angle and spine position—most people find it effective to lean forward or raise their knees, which can help the muscles around the anus to relax
- When you lean forward, place your forearms on your thighs for support
- Relax suggestions
- Breathe deeply in through your nose and out slowly through your mouth as if you are smelling the flowers and blowing out the candles.
- To become aware of how to relax your muscles, contracting and releasing muscles can be helpful. Pull your pelvic floor muscles in tightly by using the image of holding back gas, or closing around the anus (visualize making a circle smaller) and lifting the anus up and in. Then release the muscles and your anus should drop down and feel open. Repeat 5 times ending with the feeling of relaxation.
- Keep your pelvic floor muscles relaxed; let your belly bulge out.
- The digestive tract starts at the mouth and ends at the anal opening, so be sure to relax both ends of the tube. Place your tongue on the roof of your mouth with your teeth separated. This helps relax your mouth and will help to relax the anus at the same time.
- Empty (defecation)
- Keep your pelvic floor and sphincter relaxed, then bulge your anal muscles. Make the anal opening wide.
- Stick your belly out as if you have swallowed a beach ball.
- Make your belly wall hard using your belly muscles while continuing to breathe. Doing this makes it easier to open your anus.
- Breath out and give a grunt (or try using other sounds such as ahhhh, shhhhh, mooo or grrrrrrr).
4) Finish
As you finish your bowel movement, pull the pelvic floor muscles up and in. This will leave your anus in the proper place rather than remaining pushed out and down. If you leave your anus pushed out and down, it will start to feel as though that is normal and give you incorrect signals about needing to have a bowel movement.
About Fecal Incontinence
Fecal incontinence is loss of control over bowel movements. Diarrhea is short-term loss of bowel control and can happen to anyone as an isolated event. Some people experience constant loss of gas (flatus) without awareness, which is called anal (gas) incontinence. Loss of bowel control can also occur as a result of:
- childbirth or traumatic injury to the rectal area
- irritation or infection of the rectum, anus, or the surrounding area
- spinal cord injury
- brain condition such as head injury, stroke, or coma
- chronic constipation (can cause the muscles of the rectum and intestines to stretch and weaken)
- Alzheimer’s disease or other dementias
Treatment Options depend on the cause
Many people benefit from behavioral techniques and/or exercise. These include:
- exercises for the sphincters and pelvic floor muscles
- learning proper bowel health maintenance
- proper toileting positioning
- dietary factor management (increased fiber and/or water, decrease irritating foods)
- bowel retraining / learning control techniques
Surgery
In rare cases, surgery may be needed to repair the muscle at the opening of the rectum. Another type of surgery is a colostomy. A colostomy attaches part of the colon to an opening in the wall of the abdomen. Bowel movements then pass through this opening instead of the rectum. They are collected in a bag outside the body.
Medication or fiber supplements
A person can usually control stool better when it is firm rather than loose or liquid. Sometimes taking medications to change the consistency of the stool can provide relief. Using fiber supplements like Metamucil (psyllium), Konsyl, Benefiber or Citrucel to bulk the stool is a good place to start.
You may need to try over-the-counter anti-diarrhea medications such as Imodium, and prescription medications like Lomotil. These medications should be discussed with your physician prior to use.
Skin Care and Bowel Hygiene
Anyone who has frequent bowel movements, diarrhea, or bowel leakage (fecal incontinence) may experience soreness or skin irritation around the anal region. Occasionally, the skin can become so inflamed that it breaks into open sores. Prevent skin breakdown by following good skin care habits.
Cleaning and Washing Techniques
After having a bowel movement, men and women should tighten their anal sphincter before wiping. Women should always wipe from front to back to prevent fecal matter from getting into the urethra and vagina.
Tips for Cleaning and Washing
- wipe from front to back towards the anus
- always wipe gently with soft toilet paper, or ideally with moist toilet paper
- consider a bidet attachment for your toilet
- wipe only once with each piece of toilet paper so as not to re-contaminate the area
- wash in warm water alone or with a minimal amount of mild, fragrance-free soap (Cetaphil)
- gently pat skin completely dry, avoiding rubbing
- if drying the skin after washing is difficult or uncomfortable, try using a hairdryer on a low setting (use very carefully)
- allow air to get to the irritated area for some part of every day
- use protective skin creams containing zinc as recommended by your doctor
What To Avoid
- baths with extra-hot water
- soaking for long periods of time in the bathtub
- disinfectants and antiseptics
- bath oils, bath salts, and talcum powder
- using plastic pants, pads, and sheets, which cause sweating
- scratching at the irritated area
Additional Tips
- some people find that citrus and acidic foods cause or worsen skin irritation
- eat a healthy, balanced diet that is high in fiber
- drink plenty of fluids
- wear cotton underwear to allow the skin to breathe
- talk to your healthcare provider about further treatment options; persistent problems need medical attention
Bowel Control and Holding On
When bowel control is decreased or lost it is helpful to understand some control techniques. Here are some tips for controlling your bowel movements.
- Choose the best time of day to have a bowel movement:
- Usually the best time of day for a bowel movement will be a half hour to an hour after breakfast. For some people, a half hour to an hour after lunch will work better. These times are best because the body uses the gastrocolic reflex, a stimulation of bowel motion that occurs with eating, to help produce a bowel movement.
- Make sure that you are not rushed and have convenient access to a bathroom at your selected time.
- Eat all your meals at a predictable time each day. The bowel functions best when food is introduced at the same regular intervals.
- The amount of food eaten at a given time of day should be about the same size from day to day. The bowel functions best when food is introduced in similar quantities from day to day. It is fine to have a small breakfast and a large lunch, or vice versa, just be consistent.
- Eat two servings of fruit or vegetables and at least one serving of complex carbohydrates (whole grains such as brown rice, bran, whole wheat bread, or oatmeal) at each meal.
- A serving of fruit or vegetables is a half-cup or medium-sized piece of fruit. A serving of a complex carbohydrate is a half-cup or a slice of bread. It is often desirable to eat more than the recommended minimum amounts of fruits, vegetables, and complex carbohydrates.
- Drink plenty of water—ideally 4+ glasses a day.
- Until regular bowel movements are established at a desired time of day, take 2-3 dried prunes (or ¼ to 1/3 cup of prune juice) each night to stimulate morning bowel function.
- Exercise daily. You may exercise at any time of day, but you may find that bowel function is helped most if the exercise is at a consistent time each day.
Control Techniques —Relearning to control urge and bowel movements
If you are experiencing incontinence here are some techniques for controlling and resisting the urge so that you can get to the toilet without leakage.
If you are having two or three bowel movements in quick succession in the morning, you may eventually be able to hold on to the first ones, so that you have just one larger bowel movement at once. Also, when you have some successes with holding on, you become more confident, panic less, and therefore feel less urgency. The less you panic, the easier it is to make the urge go away.
Resisting the Urge
- Sit on the toilet and try to hold on for one minute before having a bowel movement. Don’t forget to take a watch or clock into the bathroom with you. Gradually increase this to five minutes. Don’t worry if you are not able to do this for the first few times, but keep practicing.
- When you have mastered this, repeat the above but hold on for ten minutes before allowing yourself to have a bowel movement. This stage is harder, but remember that you are on the toilet and are therefore “safe.”
- Once you are able to delay having a bowel movement for ten minutes while sitting on the toilet, you can begin moving away from the toilet. The next stage is to sit near the toilet when you feel the need to have a bowel movement, either on the edge of the tub or on a chair near the toilet. Hold on for five minutes. Once you are able to do this, repeat the exercise, increasing to ten minutes.
- When you are able to delay having a bowel movement for ten minutes while off the toilet, you should now gradually move further away. As your muscles are becoming stronger, you should be able to hold on for ten minutes, and as you feel more confident, increase the distance between you and the toilet.
Gradually, you will find that you can increase the distance and the time away from the toilet. This may take some time to master, but obviously the more you practice both your sphincter exercises and this program, the sooner you are likely to succeed.
***These techniques apply only if you are experiencing incontinence, otherwise you should always listen to your body signals if you feel the urge for a bowel movement.
About Irritable Bowel Syndrome
Overview
Irritable Bowel Syndrome (IBS) is a disturbance of colon function characterized by abdominal discomfort, bloating, and abnormal bowel movements. It can have either constipation or diarrhea dominance or alternate between the two. “Irritable” means that the nerve endings in the lining of the bowel are unusually sensitive, and that the nerves that control the muscles of the gut are unusually active. The bowel is more or less responsive to what might be normal events such as passing gas or having a bowel movement.
Causes
The cause of IBS is not completely understood. People with IBS have altered patterns of colon muscle contraction and hypersensitivity of the nerves in the GI system. IBS is not directly caused by stress or anxiety, but symptoms are greatly aggravated by them.
Symptoms
- abdominal bloating and gas
- chronic diarrhea
- constipation
- alternating pattern of diarrhea and constipation
- pencil thin bowel movements
- sensation of not being able to empty bowels fully
- abdominal pain or spasms, which feels relieved after a bowel movement
- nausea
Anemia, bleeding, weight loss, and fever are not symptoms of IBS, and a physician should be contacted immediately if they occur.
Treatment
IBS should be diagnosed by your healthcare provider to ensure that other medical conditions are not causing your symptoms. You may be asked to keep a daily diary to help identify diet or situations that provoke IBS.
Proper rest, diet, and exercise can help reduce stress and positively influence IBS. Treatment is not usually associated with hospitalization or surgery. Your physician may also be able to recommend medications that can help.
Tips on How to Cope with IBS
- Eat a healthy diet with plenty of water, soluble fiber and avoid high fat foods.
- Try more frequent meals with smaller portions (six times per day rather than three)
- Learn coping skills that lessen vulnerability to stressful situations, such as breathing exercises, relaxation and meditation techniques. Get help for emotional disorders such as depression, panic, or anxiety, which may make IBS worse.
Pelvic Floor Exercises for Bowel Control
Exercises using both the external anal sphincter and the deep pelvic floor muscles can help you to improve your bowel control. When done correctly, these exercises can tone and strengthen the muscles to help you hold back gas and prevent fecal incontinence (leakage of stool). Exercise programs take time; you may not see any noticeable change in your bowel control immediately. In some cases it may take several months to regain control.
Bowel Control Muscles
The anus and the anal canal, has rings of muscle around it. The outer ring of muscle is called the external anal sphincter; it is a voluntary muscle which you can learn to tighten and close more efficiently. When you contract it you will feel the skin around your anus tighten and pull in as if the anus is winking. Try to keep the buttocks muscles relaxed.
The inner ring around the anus is the internal anal sphincter. It is an involuntary and automatic muscle; you don’t have to think to keep it closed or open. This muscle should be closed at all times, except when you are actually trying to have a bowel movement.
In addition to the sphincter muscles, there are deeper muscles called the levator ani that form a sling from your tailbone to your pubic bone. The levator ani muscle has a specific part called the puborectalis that holds stool in until you give the signal to relax and empty. When you contract these muscles it creates a feeling of lifting the anus inward.
Effective Exercises for Control of Gas and Bowels
- Identify the specific areas of the pelvic floor muscles you need to use. This can be done using a mirror to see if you are contracting the correct muscles or by placing the pad of your finger at or just inside the anal opening.
- Develop an exercise plan for strength, endurance and quick response of the muscles and stick with it. You must make the muscles do more than they are used to doing.
- Incorporate the exercises into your daily activities.
Your Home Program
General Guidelines for Pelvic Floor Exercise
- Challenge your muscles to do more than they are used to doing. The quality of the exercise is more important that the number you perform.
- Avoid straining, holding your breath or using buttock or leg muscles while you exercise the pelvic floor muscles. Count out loud and continue breathing to avoid straining.
- Relax your body and breathe during your exercises. Coordinate your breathing with your pelvic floor contraction by blowing out or exhaling while you contract your pelvic floor muscles.
- Concentrate on activating both the sphincters and levator ani muscles of the pelvic floor with each exercise.
Position for the Exercises
- Start lying down with your knees bent and supported with pillows.
- Once you’ve gained awareness and can feel the contractions you may perform the exercises either sitting or standing. For example, you can do them while driving, working on the computer, or waiting in lines.
Quick Contractions
- Repeat this exercise _____ times. Do the exercise _____ times per day.
- Rapidly contract your pelvic floor muscles and hold for 2 seconds relax for 2 seconds.
- Try to do the contraction on breathing exhalation.
Endurance Contractions
- Repeat this _____ times. Do the exercise _____ times per day.
- Pull your pelvic floor muscles up and in and hold for _____ seconds then relax for _____ seconds.
- Count out loud while you are holding the contraction to make sure that you are breathing throughout the exercise and not straining.
Other Exercises/Instructions
_____________________________________________________________________________________________________________________________________________________________________________________________
High Fiber diet supplement to increase regularity:
- 1c. applesauce
- 1c. oat or wheat bran
- 1/2c. prune juice
- Combine the above ingredients. Take 1Tbsp morning and evening.
- Granola
- 4c. oatmeal
- 1 ½-2c. wheat bran/germ (or oat bran), can add flaxseed meal and/or chia
- (~1-1 ½ c bran, ¼-1/2 c flax/chia combined more or less to taste)
- 1c. shredded, unsweetened coconut
- 1 tsp cinnamon (or more to taste)
- 1/2c oil
- 1/2c honey (or molasses or maple syrup)
- 1 tsp vanilla
- Combine in large bowl, stirring well. Then add any or all of the following:
- 1c nuts (slivered almonds)
- 1c sunflower seeds
- Dried fruit (about ½-1c each) (I use currants and dried cranberries- about ¾ c each)
- Put in roasting pan or 2 large casserole pans, bake at 325 deg. for 20 min. Stir after taking out, cool, and store in airtight container. Makes about 10 cups.
- ½ c. serving has 19 g whole grain, 290 calories, 7g protein, and 5g fiber
Bowel/GI Resources
- Youtube: “How to empty your bowels without straining” Michelle Kenway, PT
- “Fiber Fueled” Dr Will Bulsiewicz MD www.Theplantfedgut.com
- “Cook for your Gut Health” America’s Test Kitchen (cooksillustrated.com)
- “Gentle Nutrition” Rachel Hartley, RD
- “The Bloated Belly Whisperer” Tamara Duker Freuman, RD
Podcast: “Lets Gut Real”, “Pursuit of Health”
Apps:
- Constipation Stool Diary; MyGIHealth; Bowelle; NERVA; MyHealthyGut; MyIBS; MySymptomsFoodDiary; MonashFODMAP; FIG; Spoonful; Poop Tracker Toilet Log; PainScale
- www.Helpforibs.com
- www.ibsdiets.org/fodmap-diet/
- www.pelvicpainrehab.com/blog look for constipation, fecal incontinence, IBS etc
- www.bebalancedrdn.com Holly van Poots, RDN in Harrisonburg
- Renew inserts (anal plug) for fecal incontinence: renew-medical.uk
FODMAP diet– used primarily for IBS as a short term elimination diet to see if you are sensitive to certain foods. The goal is to eventually return them to your diet (or know which ones to stay away from). Check with your doctor first, as there are some precautions with this diet.
- Hopkinsmedicine.org/health/wellness-and-prevention/fodmap- diet
- Gi.org/topics/low-fodmap-diet
As a general rule, if you do not have Celiac or an actual allergy to milk proteins, wheat and dairy may not need to be avoided, and the goal is to have a wide variety of food choices. For some, the A1 protein in dairy is a problem- you can find A2 milk
Foods that may increase GI symptoms:
- Processed foods
- Dairy
- Eggs
- Sugars
- Wheat/gluten- especially processed baked goods (ie white flour).
- Many people do ok with more whole grain options, or with homemade – even with white flour, or may tolerate organic better
- May also be quantity – can tolerate a little, but not a lot
Use fiber supplement (Metamucil, konsyl, benefiber, Citrucel) to bulk up loose stools, and miralax to soften hard stools as needed- you will need to experiment with this balance!
