Female Urinary Incontinence Resources
Bladder Health
What is Considered Normal?
- The bladder is a storage reservoir that sits right behind the pubic bone.
- Can hold about 2 cups (15-20 oz, or ~750ml) of urine at full capacity
- Normal average voiding time is about 2-4 hours. As we get older, the bladder gets less elastic, capacity decreases, and we need to urinate more frequently. Still usually not more often than every 2 hrs.
- Voiding more often than every 2 hrs may not allow the bladder to fill, and “trains” it to be smaller and get an urge with less volume.
- Urine should flow easily in a good, steady stream until the bladder is empty. No pushing or straining should be needed.
- Most people void about 8-12 oz in a “normal” void, and about 1oz/second, so you should urinate about 8-12 seconds.
- When about 5-6 oz of urine are in the bladder, it stretches and sends an urge signal to the brain. Most of the time, we can ignore that urge for 2+ hrs.
- Urges should not be commands to empty your bladder, just a signal to let you know it’s coming.
- Not all urges happen with a full bladder, and it can be hard to tell the difference!
What are good bladder habits?
- Take your time when emptying your bladder.
- Don’t strain or push, just let it all come out.
- You may need to jiggle or stand up/sit down a time or 2 to make sure it empties all the way.
- Try not to go more often than every 2 hrs, or “just in case”. Again, you don’t always have to go at the first urge. Wait until your bladder feels full if you can. This may take time to retrain!
- On the other hand, consistently ignoring the urge and going more than 4 hours isn’t healthy either.
- Urgency and frequency can be improved by retraining the bladder and spacing your fluid intake through the day.
Fluid Intake
- One of the first things people do if they are leaking urine or have strong urge is to not drink as much so they won’t have to pee as much.
- Look at how much you are drinking. For instance, if you’ve just had 2 c coffee, a glass of water with your meds, and then a glass of juice, no wonder you have an urge- that’s a quart of liquid!
- So slow it down. Try drinking the same amount over a longer period of time
- Urinary leakage is not an intake problem as much as a storage problem.
- Our bodies need fluid. We are about 90% water. While there is no scientific evidence to support the 8 glasses (64 oz) of water a day, we do need enough to stay hydrated.
- Normally, urine should be pale yellow and have minimal odor. Some medications can change color and odor, so this is not set in stone.
- Most people urinate more in the morning- you haven’t gone as often overnight, moved around less, and then start moving around and have something (often caffeinated) to drink. All of this increases the volume of urine in your bladder, and it is normal to need to urinate often for the first several hours in the morning.
Constipation
What does constipation have to do with urinary leakage?
- Not enough water intake can make stools hard (need about a quart a day)
- Stool in the colon can put pressure on the bladder, increasing urgency
- Straining to have a BM can increase risk of hemorrhoids and weaken the muscles
It is possible to have regular BM or even loose stools and still be constipated. If you have a BM (often fairly well formed), then several hours later have a little more- maybe more pebble shaped, and then some loose, liquidy stool or even smearing, this may be the liquid part oozing around a harder stool up in the rectum/colon.
- Despite what your mom told you, you don’t necessarily need to have a BM every day.
- Some people’s digestive systems just move a little slower.
- You should have a “soft, fluffy” stool that is easy to pass without straining.
- You shouldn’t ignore the urge to have a BM. While you don’t always need to go right then, don’t get in the habit of putting it off too long.
- Retrain your system to go at a more convenient time. It is easiest to have a BM about 20-30 min after a meal, as what you just ate stimulates waves of muscle contractions through the intestines to move the food along. The strongest is in the morning.
- Need about a quart of water a day for good stool consistency
- The longer stool sits in the colon, the more water gets absorbed out, and the harder it gets
When the stool gets down to the rectum, a little bit comes down into the anus and is “sampled” for consistency. The nerves know the difference between liquid, gas, and solid stool. Gas and solid should be able to be held for a little while. The strongest sphincter in the world can’t hold liquid (diarrhea) for more than a few seconds- so find a bathroom fast.
How Diet Can Effect Your Bladder
The following foods may irritate the bladder when consumed in large amounts. Not all of these affect everyone- so it may be some trial and error!
- Alcohol: Reduce to 0-1 drink per day.
- Caffeine (in any caffeinated beverage and some medications): Reduce to 0-1 per day.
- Acid fruit and fruit juices (orange, grapefruit, cranberry, tomato)
- Tomatoes and products containing tomatoes
- Spicy foods
- Milk products
- Raw sugar and added sugar
- Carbonated Beverages: Reduce to 0-1 per day.
- Artificial Sweeteners
Medications that may cause temporary urinary incontinence or make existing incontinence worse, but this doesn’t mean you should go off any of them- just may be harder to gain full control:
Antihistamines Diuretics Anti-psychotics
Sleeping Pills or Sedatives Antispasmodics Decongestants
Anti-Parkinson Agents Antidepressants Calcium Channel Blockers
Be sure to drink enough liquid (water is best). Urine should be clear to pale yellow and have minimal odor if you are well hydrated. Caffeine and alcohol are diuretics- pull fluid from your system and make more urine.
Pelvic Floor Muscles
The pelvic floor muscles form the base of the pelvis and support the pelvic organs (rectum, bladder, uterus) and the abdominal contents from above. They act like a trampoline to give support against pressure from above, and “close off the hose” of the urethra and the anus to stop (or start) urine/feces. These muscles work both automatically (we don’t usually have to think about stopping the flow of urine) and voluntarily (we can stop the flow of urine).
- When they get weak, they generally can’t contract strongly enough to stop the flow of urine- the trampoline “gives” too much. This may also result in prolapse where the bladder, uterus, or rectum “drop” into the vaginal wall. Weakness often begins during pregnancy and the stretching with delivery, but many people who have never had children have leakage.
- Sometimes when the muscles are weak, they will work extra hard to do their job and get tight or spasmed and painful. In this case, we may need to work on relaxing them first before working on strength. The trampoline doesn’t give enough.
- Stress incontinence is leakage of small amounts of urine with cough/laugh/sneeze etc.
- Urge incontinence is leakage of medium amounts with strong urge- often because the muscles aren’t strong enough to stop the flow, so we empty more frequently “just in case”
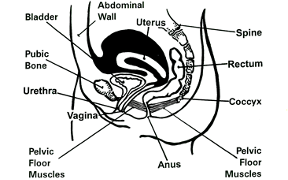
Anatomy of Pelvic Floor Muscles
The pelvic floor consists of several layers of muscle and fascia. For practical and exercise purposes the muscles can be thought of containing both a superficial (surface or exterior) and deep (inside or interior) layers.
A normal contraction of the pelvic floor can be felt both in the surface layer (urogenital and anal sphincter muscles) and deeper inside layer (levator ani muscles) during a contraction. It can voluntarily contract, relax and even bulge or expand to deliver a child or have a bowel movement.
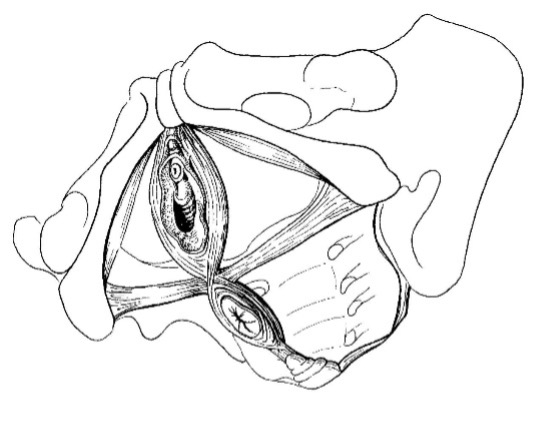

The surface muscles that surround the anal and urethral regions form a figure of 8 around the openings. When contracted they “close the openings”. In women, a tension around the vagina is noted, and the anus puckers and tightens. These are the muscles used to quickly stop the flow of urine with urge, or with cough/laugh/sneeze.
The deep muscles fill in the pelvic basin or bowl and span the width and breadth of the pelvis. They have been traditionally called a hammock, but more correctly they form an inferior floor or trampoline that attaches to a fixed frame- the bones of the pelvis. When contracted you feel a deep tension and the tailbone moves towards the pubic bone. These are your more postural muscles- they hold your organs in all day long.
A deep lower abdominal (transverse) muscle contraction can and should accompany a pelvic floor muscle contraction. This can be felt as a slight deep tension and pulling in of the lower abdomen.
Gluteal squeeze (clenching your butt cheeks) should also involve a pelvic floor muscle contraction, though you should also be able to contract PF without glutes.
The Core and Abdominals
The trunk is a cylinder with the diaphragm at the top, abdominal and back muscles around the middle, and pelvic floor on the bottom. All muscles must work together to distribute pressure and load across the trunk. If one part of the cylinder is weak, pressure pushes out there. This cylinder is commonly also known as the “core”. The deepest of the 4 sets of abdominal muscles is the transverse abdominis, and contraction of this muscle creates a “drawing in” of the lower abdominal wall. Regular exercise of the core muscles including the pelvic floor should build strength, awareness, coordination and retrain the muscles how to function together. This in turn can be the key to controlling your incontinence problem. The core contractions create an internal girdle to support your bladder and pelvic organs as well as your back/trunk. If you hold your breath and push down and out with activity, you are also going to push urine down and out. If you activate the PF muscles and core, the muscles can counteract the pressure from above, and urine stays put.
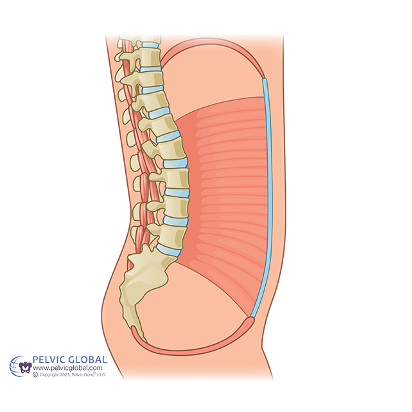
- Strong /well-coordinated abdominal muscles (core) aid the pelvic floor in its function of positioning the urethra and bladder into the pelvic cavity.
- Contracting the abdominal and pelvic floor muscles before and during a cough (or other activity that increases pressure) decreases pelvic floor bulging and urinary leakage.
- Abdominal muscles must work with – not against – the pelvic floor muscles and should be contracted without holding your breath.
- Breathing patterns can affect the system as well. Normally as the diaphragm lowers during an inhale, the pelvic floor muscles lengthen slightly. Normal exhale is passive, and on forced exhale, both abdominals and PF muscles contract (think blowing out birthday candles).
- The pelvic floor muscles and lower abdominals (transverse abdominis) should normally contract together during all activities, especially lifting.
Pelvic Floor Muscle Contractions (aka Kegels)
Pelvic muscle contractions are used to strengthen the muscles to prevent urine leakage and decrease urgency. They can/should be done while sitting, standing, or lying down.
How to find the muscles:
- Imagine you are in a crowded room and you feel the need to pass gas.
- Try not to pee/try to stop the flow of urine
- Imagine pulling the vagina up inside
Common errors:
- Breath holding: If you are holding your breath, you may be bearing down against your bladder instead of pulling it up. If your belly bulges up/out while you’re squeezing, you are holding your breath. Try to breathe out gently while performing your PF exercises. This should help encourage those muscles to contract.
- Overdoing it: If you have done too many or held each squeeze too long, your muscles will fatigue and stop working for you. You may actually leak more or feel soreness at the lower abdomen, low back, or rectum.
Quick flicks. Squeeze the muscle as quick and as hard as you can for one second. Let go for one second.
Long Holds. Squeeze the muscle and hold it. You may need to retighten periodically. Rest between each one, twice as long as you held.
Aggravators. Squeeze your pelvic floor muscles during any activity which would normally make you leak (cough, sneeze, lift, getting out of bed or a chair).
Also do 5-6 quick squeezes with urge to decrease the urge before you walk to the bathroom.
Remember: “Squeeze before you sneeze.” Also known as “the knack”
| Reps. | Hold time | Rest time | |
| Quick flicks | |||
| Long Holds |
Repeat this set of quick flicks and long holds 3-6 times each day.
Work up to 6 sets of 10 quick and 10 long holds per day in standing with emphasis on the front muscles
Do in any position (sitting, standing, lying)
Challenge your muscles to do more than they are used to doing! Quality is more important than quantity.
Relax and keep breathing during exercises. These muscles are supposed to function automatically.
It may take 3-6 months to really strengthen the muscles, so don’t give up!
Overcoming the Urge
Possibly the hardest thing to relearn is to delay the need to urinate. By this point your brain is convinced that if you don’t urinate right now, you will urinate all over yourself, and the muscles may be weak enough that they can’t effectively hold it back, either. The following steps should help, but remember, this didn’t start overnight, and will not go away overnight, so don’t get discouraged and give up, it will get better if you work at it.
When you experience a strong urge to urinate:
- Stop activity, stand quietly or sit down. Try to stay still to maintain control. Avoid rushing to the toilet.
- Contract your pelvic floor muscles by squeezing and letting go 5 to 6 times to decrease the urge. Pelvic floor contractions send a message to the bladder to relax and hold urine.
- Try to distract yourself by thinking of something other than going to the bathroom. (count backwards from 100 by 7’s)
- Relax. Do not rush to the toilet. Take a deep belly or diaphragmatic breath and let it out slowly. Let the urge to urinate pass by using distraction techniques and positive thoughts.
- Rushing jiggles the bladder, so try to walk normally
- If the urge returns, repeat the above steps to regain control. When you feel the urge subside, walk normally to the bathroom. You can urinate once the urge has subsided.
Urge feeling! -> Stop and be still. -> Do not rush to the toilet. -> Think Positively -> Begin PF Contractions. -> Distract Yourself
Sleep Longer
As your body ages the bladder may become less elastic and therefore be less able to stretch to accommodate urine. It will signal the urge to void more frequently. Also, as you age your veins may become less efficient at pumping fluid from your arms and legs up toward your heart while you are upright during the day. At night when you lie down and remove the effects of gravity, your veins are better able to pump the fluid into your system where it can be converted to urine. Therefore, you will fill your bladder more frequently during the night. If you are on medications that increase urine production (diuretics), this may also cause you to need to void more frequently at night
For a better chance at getting up less frequently to void through the night:
- Limit fluids after 6 pm (or 3-4 hrs before bed).
- Especially limit caffeine or alcohol as they are both diuretics (make more urine)
- Take medications that are known to be “water pills” or diuretics as early in the day as permitted by your physician.
- Two hours before bed: Lie down with your legs above your heart while supported on pillows.
- Make circles with your ankles 20 times in each direction.
- Pump your ankles up and down 20 times.
- Straighten your knees one at time by lifting each foot up toward the ceiling and then back down to the pillow. Repeat 10 times each leg.
All information adapted from Progressive Therapeutics handouts, pelvicpainrehab.com blogs, myPFM.com, continuing education course notes
Prolapse
Prolapse happens when the pelvic organs lose their support and start to drop. You may have heard this as a “dropped bladder”. It can also happen to the uterus or rectum.
- #1 risk factor for prolapse is delivering a baby
- Feeling of pressure, heaviness or “falling out feeling” by evening or with lifting
- Tends to worsen after menopause as all tissues become less elastic
- Holding your breath to lift or straining (pushing “down and out”) can make it worse.
- Using your core and pelvic floor muscles to hold “up and in” instead of pushing “down and out” can help keep it from worsening
- A pessary can help support the walls of the vagina and keep the prolapse in place
- With a rectocele, some people need to splint the wall of the vagina to empty the rectum
- Surgery is commonly done when the prolapse is very bothersome, a pessary hasn’t worked, or it extends beyond the vaginal opening.
RESOURCES
Books:
- “The Core Program”, Peggy Brill, PT. Bantam Books, 2001. ISBN 0-553-38084-2
- “Women’s Waterworks”, Pauline Chiarelli, PT
- “The V Book: A Doctor’s Guide to Complete Vulvovaginal Health.” Elizabeth Gunther Stewart, Paula Spencer, Bantam Books, 2002
- “Come as You Are” Emily Nagoski PhD.
- “The Period Repair Manual” Lara Briden, ND
Websites:
- www.pelvicpainrehab.com/blog – numerous blog posts written for patients
- www.mypfm.com –excellent short video on “the Basics” of PF mechanics (on YouTube- “myPFM”)
- www.phoenixpub.com books on pain, fibromyalgia, incontinence, physiological quieting CD
- www.yourpaceyoga.com –website for pelvic pain specific yoga techniques
- www.pelvicpain.org –International pelvic pain Society
- www.facebook.com/groups/pelvicpain/ -multiple FB groups- Pelvic Pain Support, Nancy’s nook (endometriosis), Pelvic pain help, Interstitial cystitis 101, IC today; Fitness Return with Pelvic Organ Prolapse (also poweroverpop.com)
- www.integrativewomenshealthinstitute.com –Jessica Drummond, PT- more holistic, nutritional focus to managing pelvic pain, chronic pain…
- www.voicesofpfd.org
- www.thegreatwallofvulva.com
- www.pelvicfloorexercises.com.au
- www.suecroftphysiotherapist.com
- www.juliewibept.com both print and video blogs. Lots of info for return to running/high impact. YouTube channel (JulieWiebe), “The Diaphragm and out Internal Pressure System”, “Fit Floor part 1,2,3”
- http://choosingtobemindful.com/index.html
Apps:
- Insight timer- has guided meditation with different themes from 2-40 min
- Allura- meditation
- Breathe2relax; Calm; Headspace
- Vesica- voiding diary
